Celebrating
20 years ago, NuVasive set out to improve patient care and make less-invasive spine surgery more reproducible. Partnering with the best spine clinicians from around the globe, NuVasive developed and validated rote procedural steps, introduced technologies like NVM5 to enable surgeons through intraoperative neuromonitoring, continued to innovate throughout a procedurally integrated portfolio of access, interbody, fixation, biologics and enabling technologies, and introduced world-class training and education programs to ultimately create what we believe is the best procedure in spine, XLIF.
Today, with ~300,000 procedures performed, 200+ dedicated educational courses hosted, 500+ peer-reviewed publications and 60+ products launched, XLIF guides our continued procedural innovation and our vision of intelligent surgery.1
Click and drag on images to interact with the slider above
Clinically validated at L4–L5 and above
XLIF is effective and reproducible at addressing pathologies at L4–L5 and above from the lateral decubitus position. Clinically validated, with over 500 peer-reviewed articles,1 XLIF has demonstrated more predictable outcomes than traditional posterior spinal fusion procedures, with substantially fewer complications.2-6
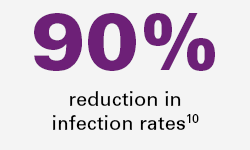
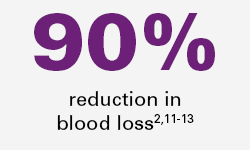
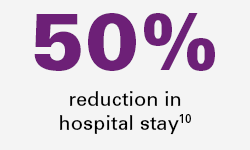
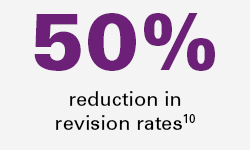
Reproducible outcomes
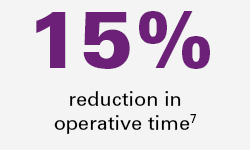
15%
reduction in operative time7
90%
reduction in infection rates10
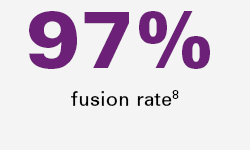
97%
fusion rate8
90%
reduction in blood loss2,11-13
50%
reduction in revision rates10
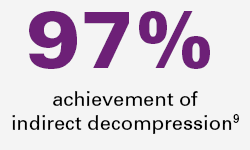
97%
achievement of indirect decompression9
50%
reduction in hospital stay10
XLIF changes lives
XLIF can provide patients shorter hospital stays and improved clinical benefits2-10, ultimately getting them back on their feet sooner.
Comprehensive procedural solution
NuVasive provides a comprehensive procedural portfolio including XLIF, XLIF- Thoracic, XLIF Corpectomy, and XLIF Crestline all accompanied by application-specific access, interbody implant, biologic, fixation solutions and enabling technologies allowing surgeons to address numerous pathologies with one surgical approach.
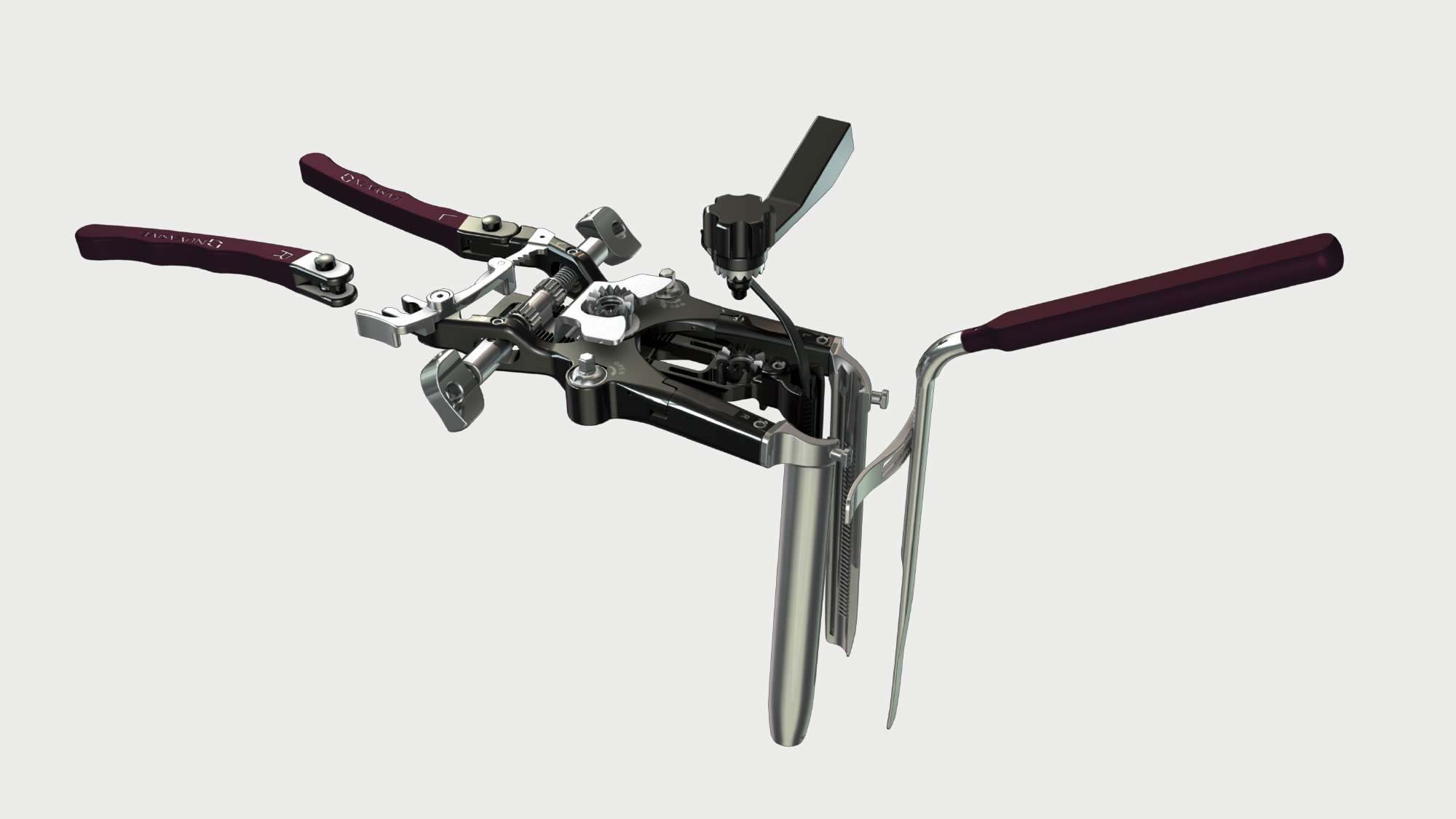
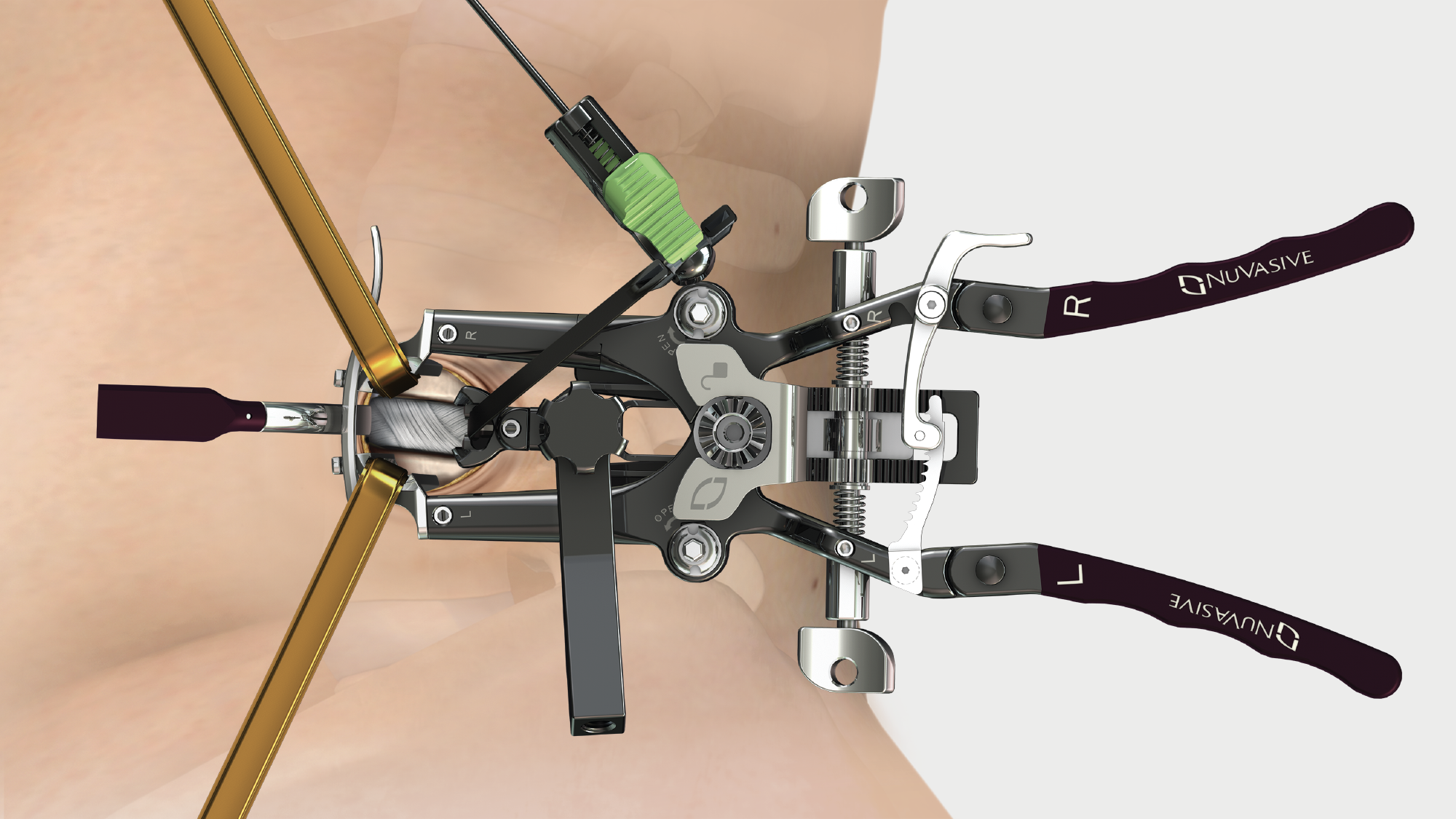
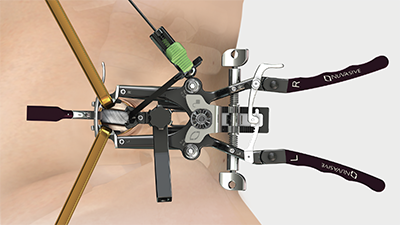
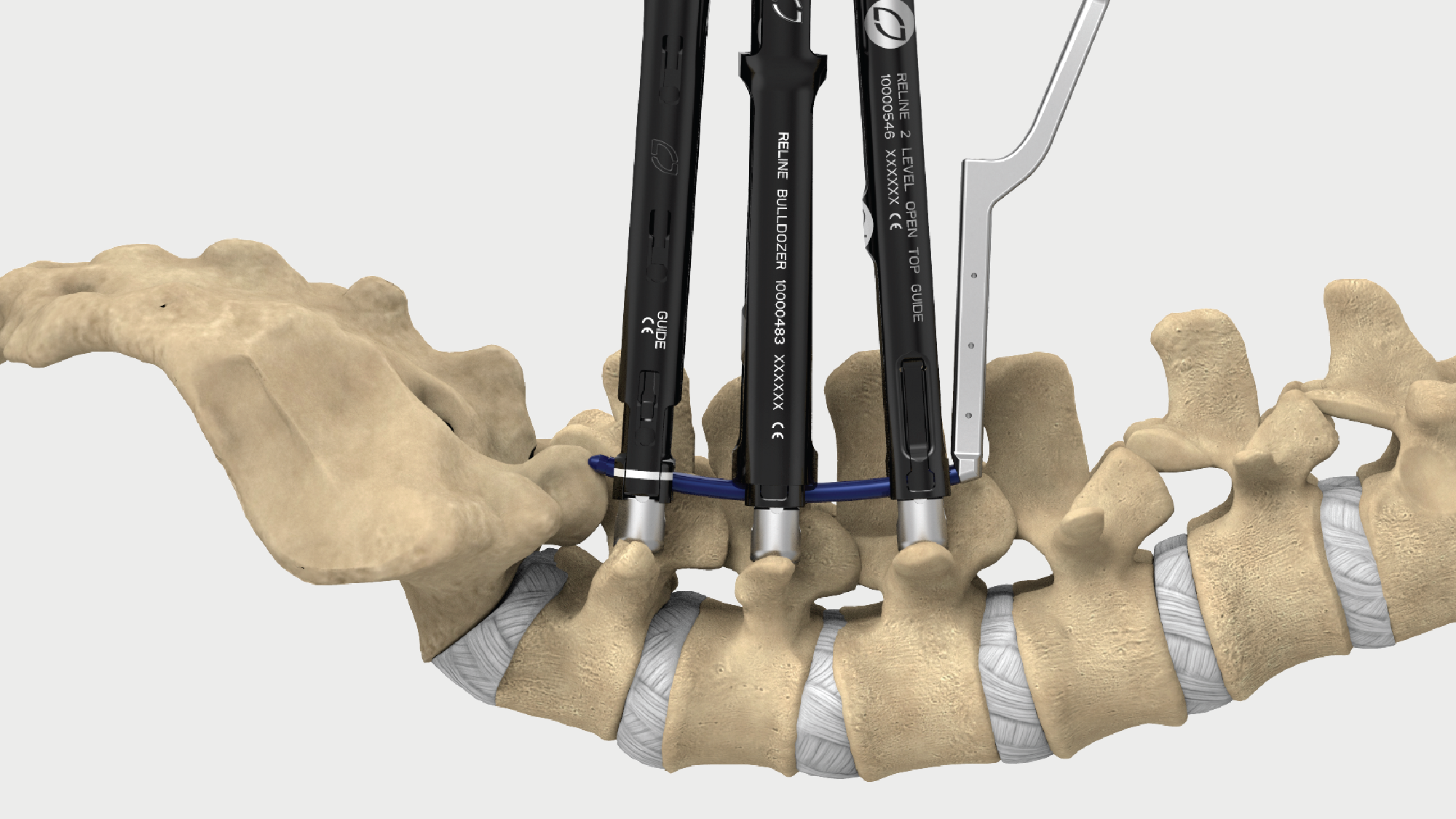
Maxcess 4
MaXcess 4 access system combines stability, ergonomics and strength to enable optimized access to relevant anatomy, while decreasing unnecessary tissue retraction. Integrated with Pulse and NVM5 neuromonitoring, Maxcess 4 provides real-time discrete thresholds, directionality and relative proximity to guide surgeons throughout the procedure from traversing the psoas through closure, providing clinically validated reproducible access at L4-L5 and above.
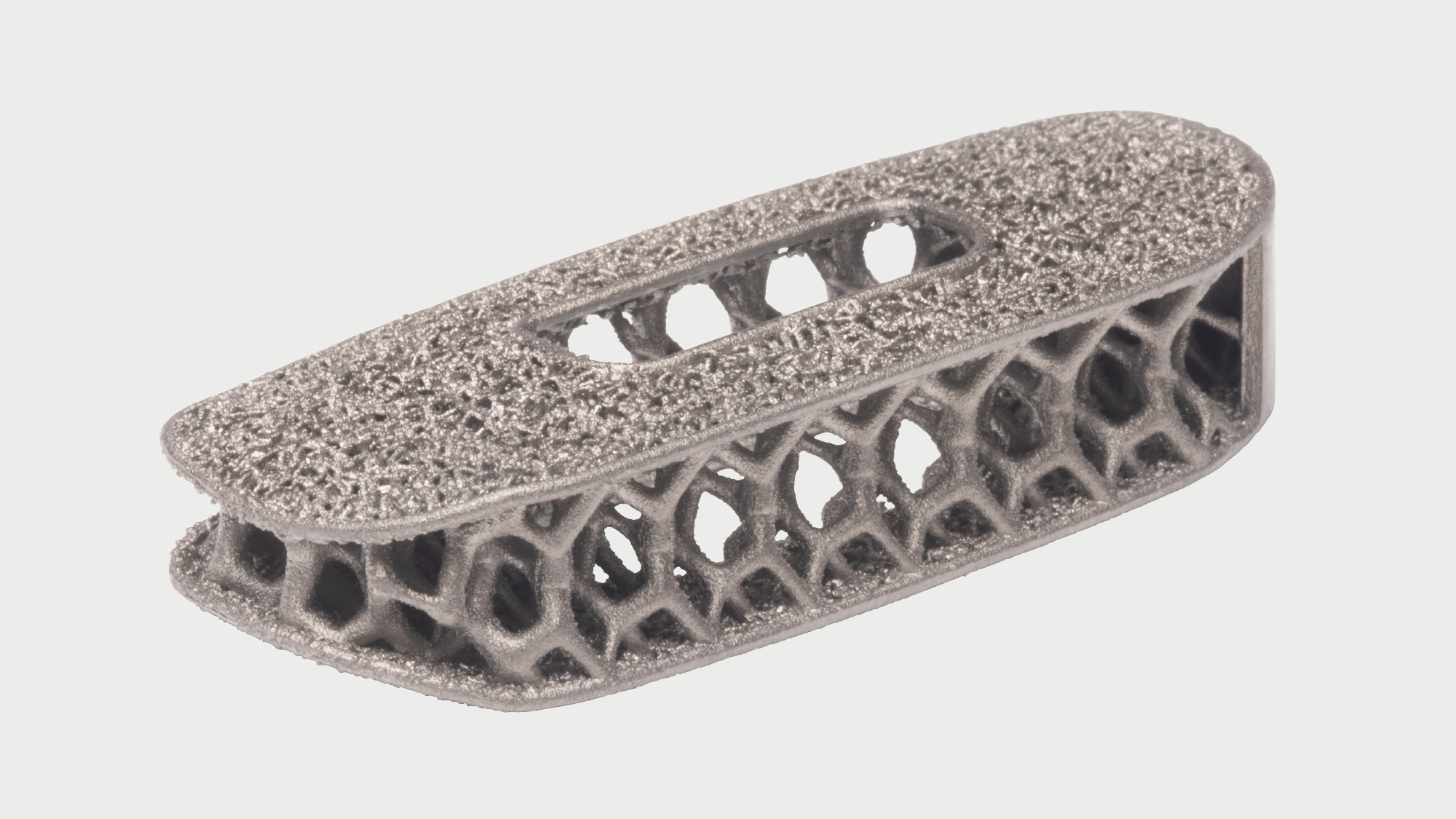
Modulus
Market-leading design integrates endplate porosity with an optimized body lattice structure.
Modulus proprietary technology integrates endplate porosity with an optimized body lattice structure providing an average porous architecture of 73% and favorable environment for bone in-growth.14

Cohere
Designed for fusion. First and only porous architecture in a radiolucent polymeric implant.
Porous endplate design promotes new bone on-growth and in-growth,15,16 leading to greater integration strength than smooth PEEK.15,17
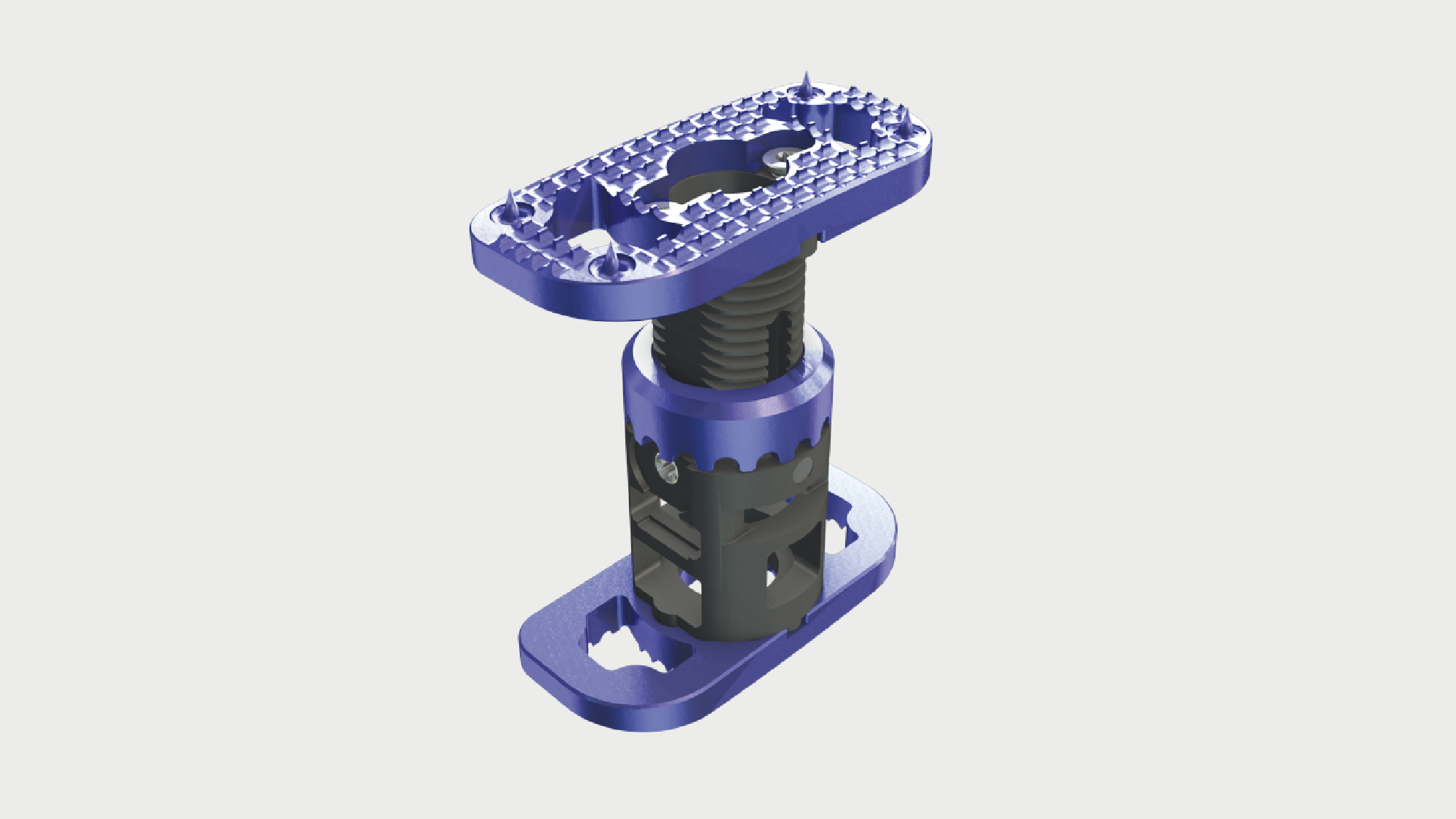
XCore 2
XLIF endcaps—increased resistance to subsidence.
The second generation XCore 2 VBR has XLIF style endcaps that are specifically designed to span the ring apophysis. Clinical data shows that XLIF endcaps of the XCore 2 VBR provide an increased resistance to subsidence as compared to cylindrical VBRs.18,19
Attrax
Attrax Putty is now the first and only synthetic biologic to receive 510(k) clearance for use with thoracolumbar interbody systems. When used with Modulus XLIF interbody implants the combination of Attrax and Modulus resulted in a 97.8% rate of bone bridging20
Learn more about Attrax

Osteocel
Osteocel is a comprehensive bone graft developed to mimic the properties of a patient's own bone. Osteocel provides a complete and physiologic bone graft that contains all of the necessary components for bone growth: the cells, the signals, and the scaffold.
Learn more about Osteocel
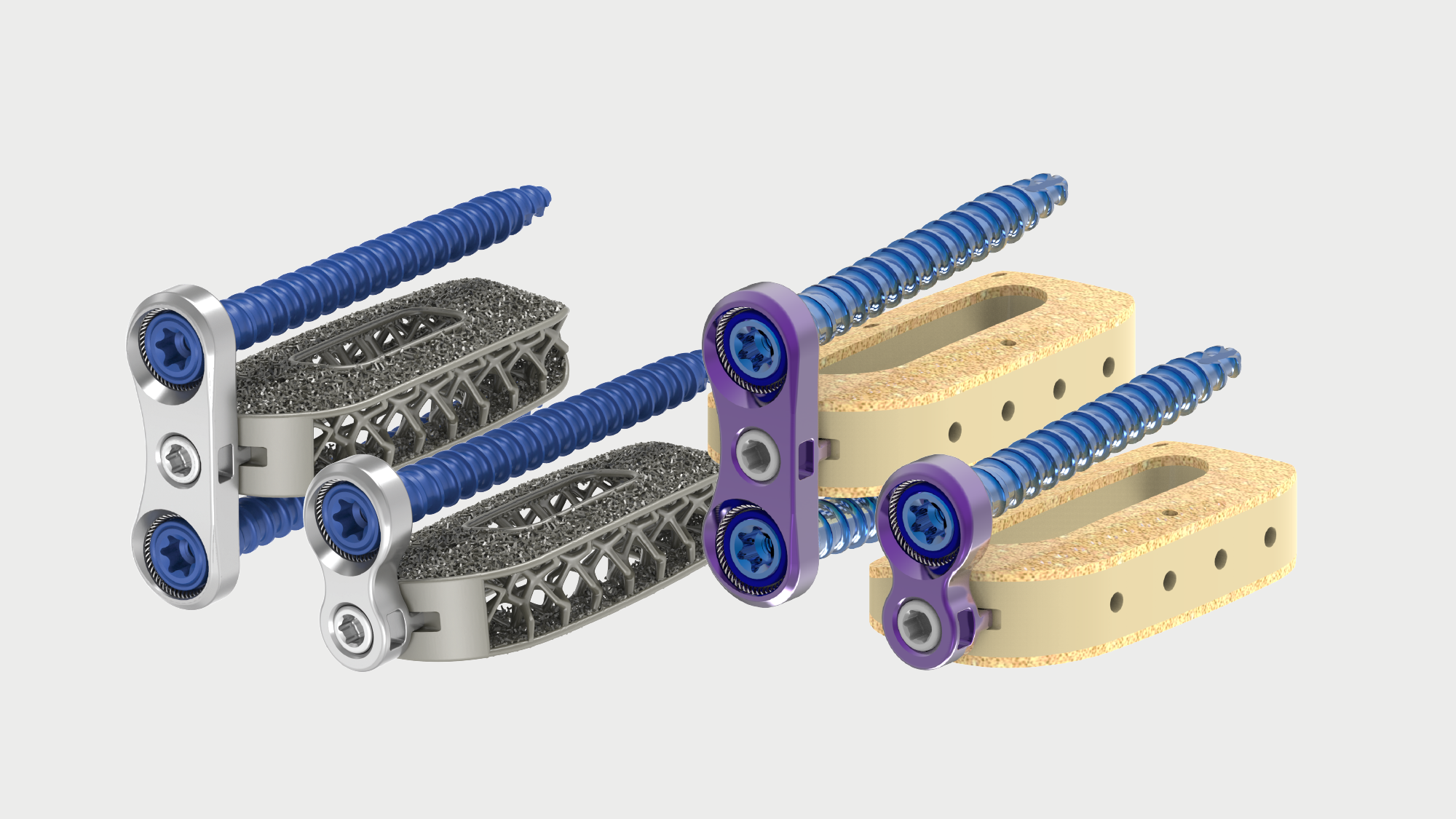
Modulus XLIF plate and Cohere XLIF AMS plate
Stability at the discretion of the surgeon, in multi-stage procedures or as standalone fixation. Simplified instrumentation allows the plates to be placed before or after insertion of the implant. The plates are available in single- and dual-sided options to best fit the surgeon and patient need.
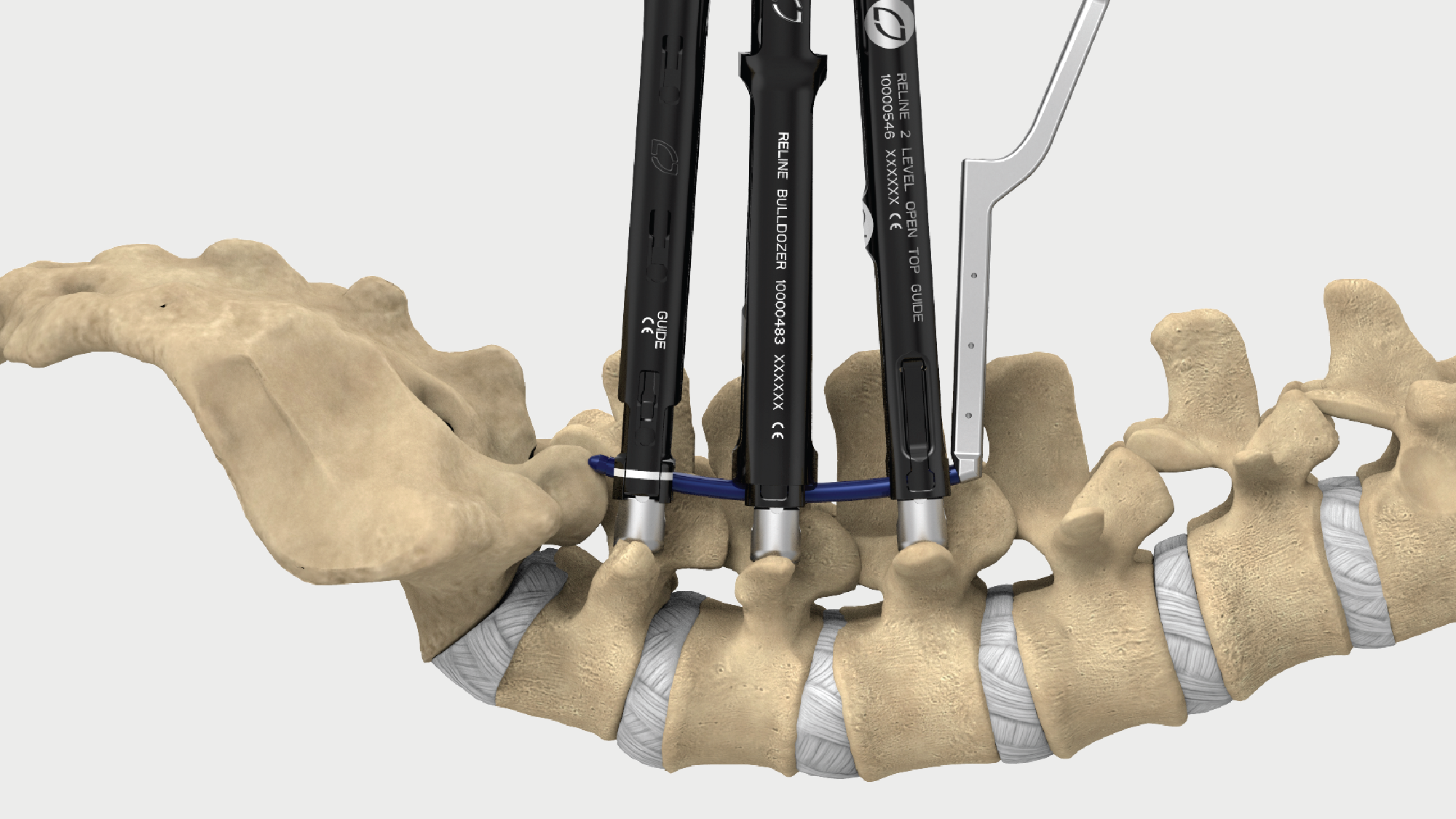
Reline
Reline is the most comprehensive fixation system in spine, offering an easy-to-use yet powerful system. Reline delivers innovative technologies to support less invasive, open and hybrid techniques in a single seamless platform.
Learn more about Posterior Fixation

Pulse
Pulse is the first solution to integrate all the technologies required to enable better spine surgery into one single platform. Pulse integrates multiple enabling technologies, like neuromonitoring, patient-specific rod bending, smart imaging with radiation reduction and navigation to improve workflow, reduce variability and increase the reproducibility of surgical outcomes.
Learn more about Pulse

Neuromonitoring
Neuromonitoring with NVM5 is a foundational requirement in every XLIF case. Our services and technology provide proprietary automated nerve detection with standardized setup and clinically validated alerts21 to help reduce variability and allow for faster interpretation of neural information.
Learn more about NVM5

Patient-specific rod bending
The Bendini spinal rod bending system is used to create customized rods which are bent exactly to XLIF interbody implant locations. The system expedites manual rod manipulation via computer-assisted bend instructions.

Lessray
The use of X-ray imaging in MIS has greatly enhanced visualization. X-ray imaging is correlated with radiation exposure, which has been shown to have a negative impact on health through repeated exposure.22 The Lessray technology was designed to increase OR efficiency through streamlined imaging workflow, while also significantly reducing exposure to radiation for everyone in the room.23
Learn more about Lessray
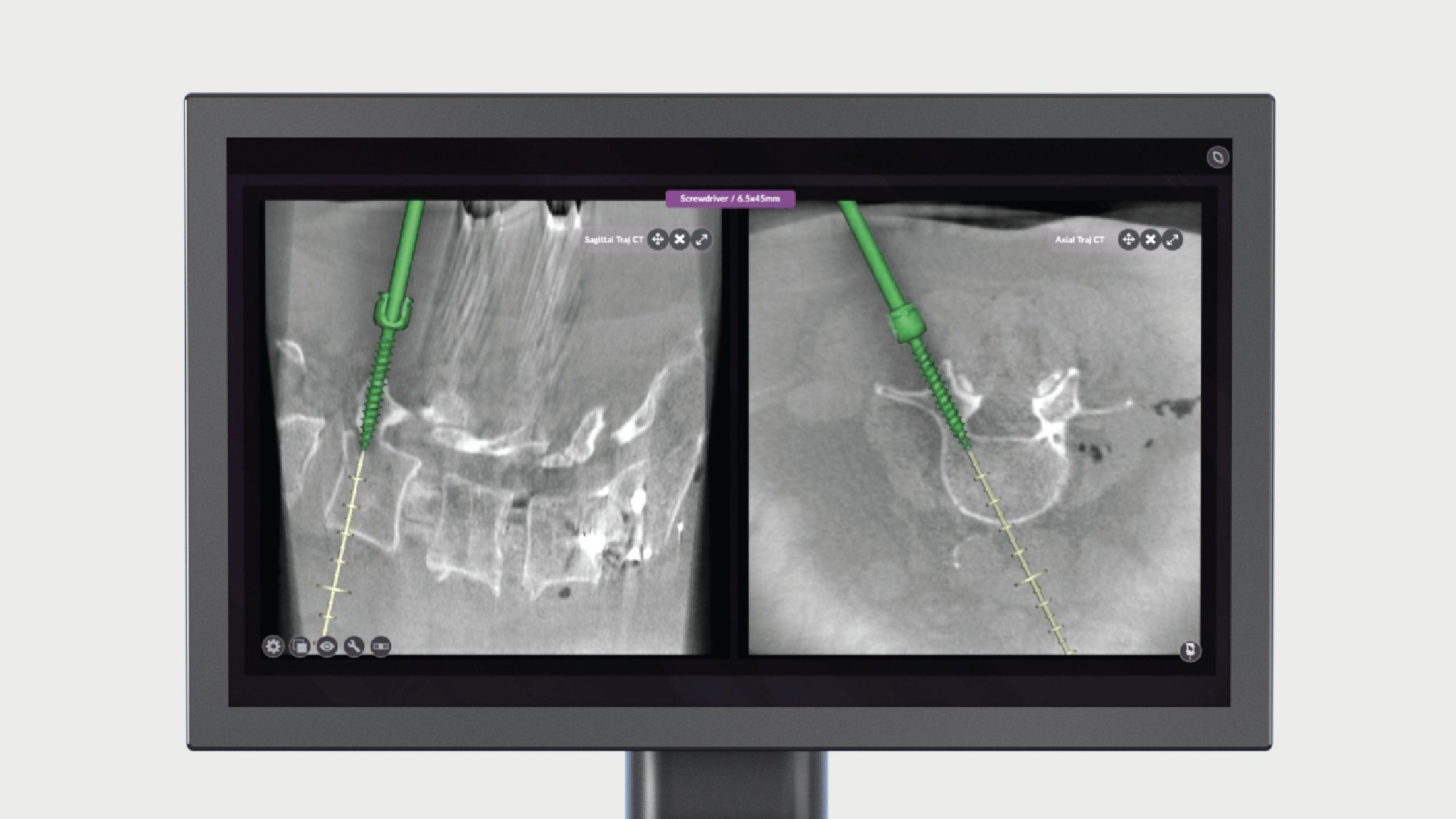
Navigation
Navigation in spine surgery offers the potential for more surgeons to adopt MIS techniques while improving implant accuracy and minimizing radiation. However, the complexity and time requirements of existing solutions have impeded adoption of navigation into the majority of spine surgeries. Pulse introduces a procedurally integrated navigation technology that features workflow technologies to improve ease-of-use and surgical efficiency in the OR.
Celebrating 20 years of XLIF
20 years ago, NuVasive set out to improve patient care and make less-invasive spine surgery more reproducible. Partnering with the best spine clinicians from around the globe, NuVasive developed and validated rote procedural steps, introduced technologies like NVM5 to enable surgeons through intraoperative neuromonitoring, continued to innovate throughout a procedurally integrated portfolio of access, interbody, fixation, biologics and enabling technologies, and introduced world-class training and education programs to ultimately create what we believe is the best procedure in spine, XLIF.
Today, with ~300,000 procedures performed, 200+ dedicated educational courses hosted, 500+ peer-reviewed publications and 60+ products launched, XLIF guides our continued procedural innovation and our vision of intelligent surgery.1
It’s been quite a journey since I started working with NuVasive in 2001, being attracted to the vision of making spine surgery better. In collaboration with a handful of my peers and the NuVasive team, creating the XLIF procedure was a decision that stemmed from us realizing that the outcomes we were seeing weren’t good enough.
This proven innovation is an incredible example of how thoughtful procedural design and reliable, reproducible clinical results can improve the overall care experience.”
Dr. Frank Phillips
Director of the Division of Spine Surgery
Rush University Medical Center
"Someone asked me, what was my ‘a-ha’ moment that really bought to light what a great procedure this was? It wasn’t in the operating room. For the first time in my entire career, a patient I operated on with a lumbar fusion referred a patient to me, rather than saying “oh, you never want to have surgery”.
I’ve had referrals from Neurologists, pain management doctors, family doctors, but do you know who refers more patients to me? Patients who have had prior XLIFs—that says a lot.”
Dr. William Smith
Neurosurgeon
University Medical Center Southern Nevada
Clinically validated at L4–L5 and above
XLIF is effective and reproducible at addressing pathologies at L4–L5 and above from the lateral decubitus position. Clinically validated, with over 500 peer-reviewed articles,1 XLIF has demonstrated more predictable outcomes than traditional posterior spinal fusion procedures, with substantially fewer complications.2-6
Reproducible outcomes
Comprehensive procedural solution
NuVasive provides a comprehensive procedural portfolio including XLIF, XLIF- Thoracic, XLIF Corpectomy, and XLIF Crestline all accompanied by application-specific access, interbody implant, biologic, fixation solutions and enabling technologies allowing surgeons to address numerous pathologies with one surgical approach.
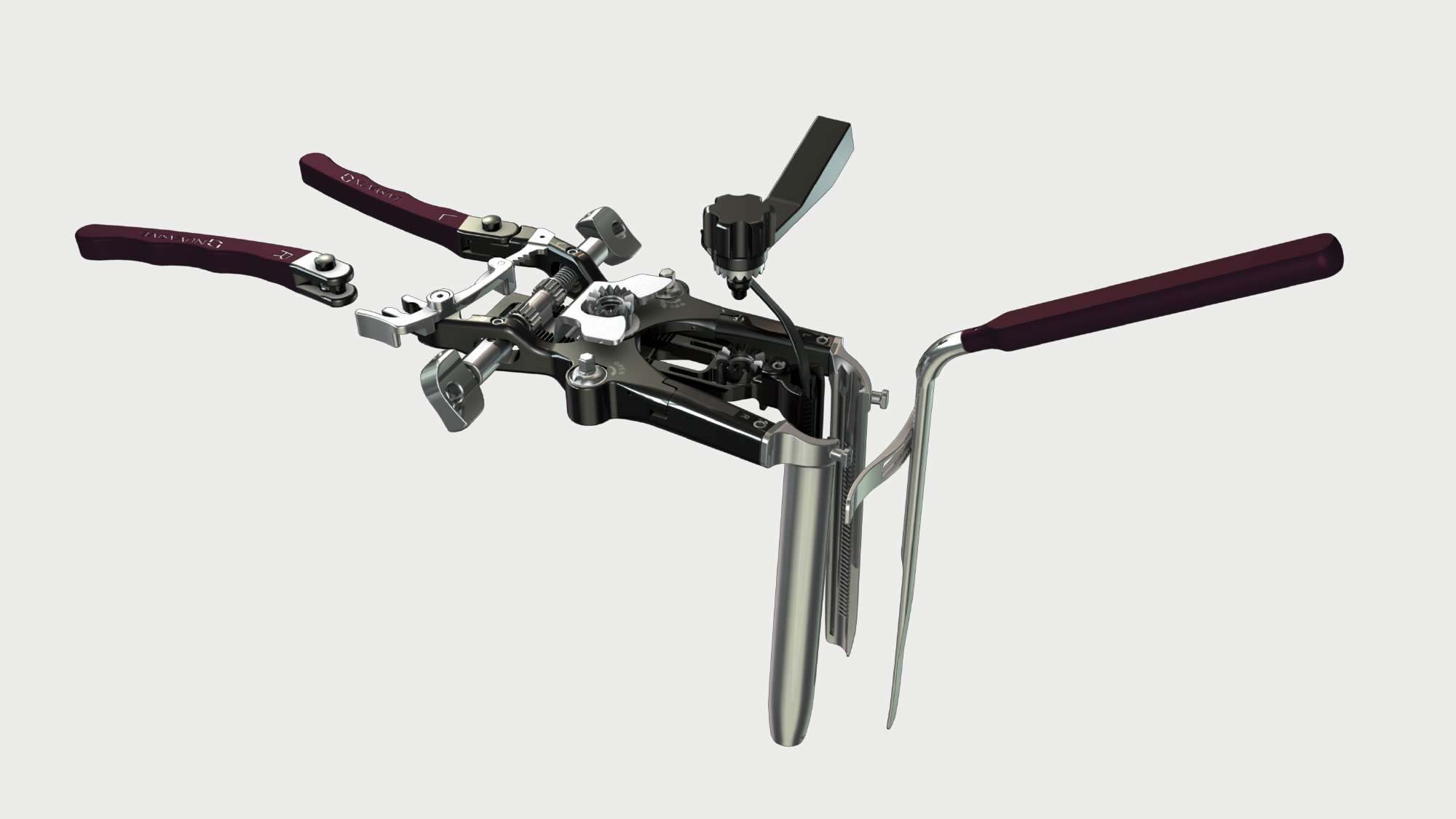
Maxcess 4
MaXcess 4 access system combines stability, ergonomics and strength to enable optimized access to relevant anatomy, while decreasing unnecessary tissue retraction. Integrated with Pulse and NVM5 neuromonitoring, Maxcess 4 provides real-time discrete thresholds, directionality and relative proximity to guide surgeons throughout the procedure from traversing the psoas through closure, providing clinically validated reproducible access at L4-L5 and above.
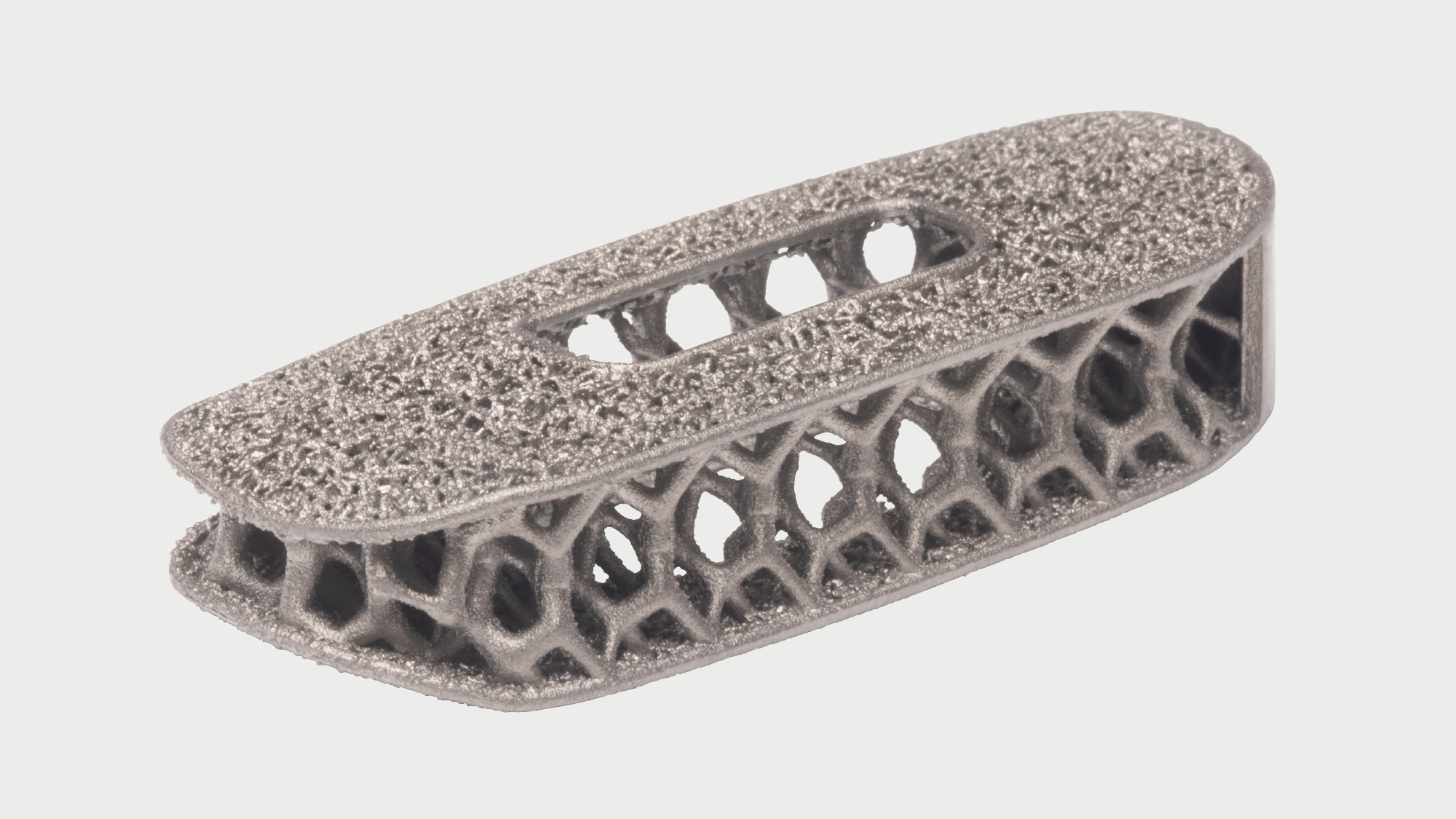
Modulus
Market-leading design integrates endplate porosity with an optimized body lattice structure.
Modulus proprietary technology integrates endplate porosity with an optimized body lattice structure providing an average porous architecture of 73% and favorable environment for bone in-growth.14

Cohere
Designed for fusion. First and only porous architecture in a radiolucent polymeric implant.
Porous endplate design promotes new bone on-growth and in-growth,15,16 leading to greater integration strength than smooth PEEK.15,17
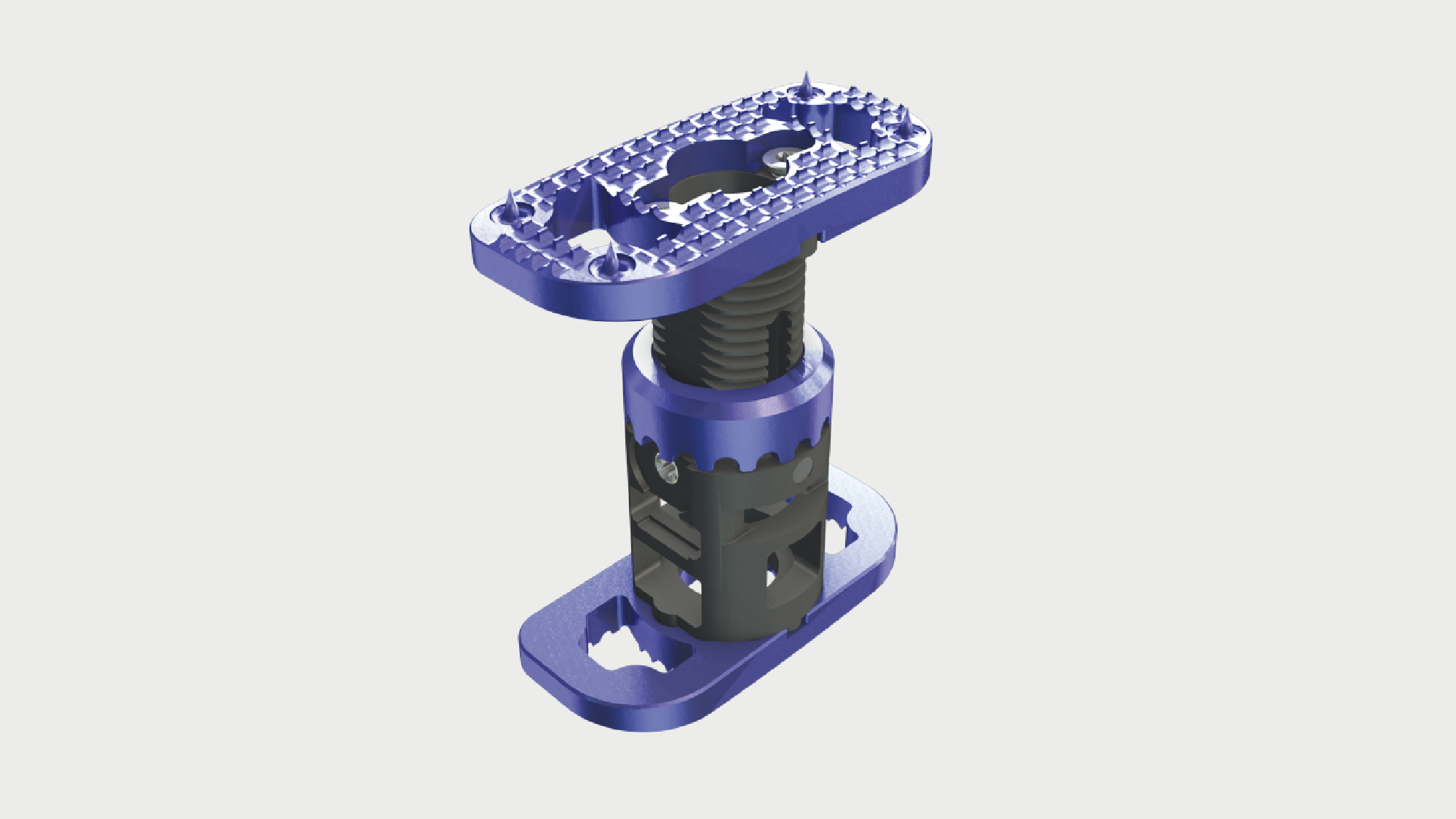
XCore 2
XLIF endcaps—increased resistance to subsidence.
The second generation XCore 2 VBR has XLIF style endcaps that are specifically designed to span the ring apophysis. Clinical data shows that XLIF endcaps of the XCore 2 VBR provide an increased resistance to subsidence as compared to cylindrical VBRs.18,19
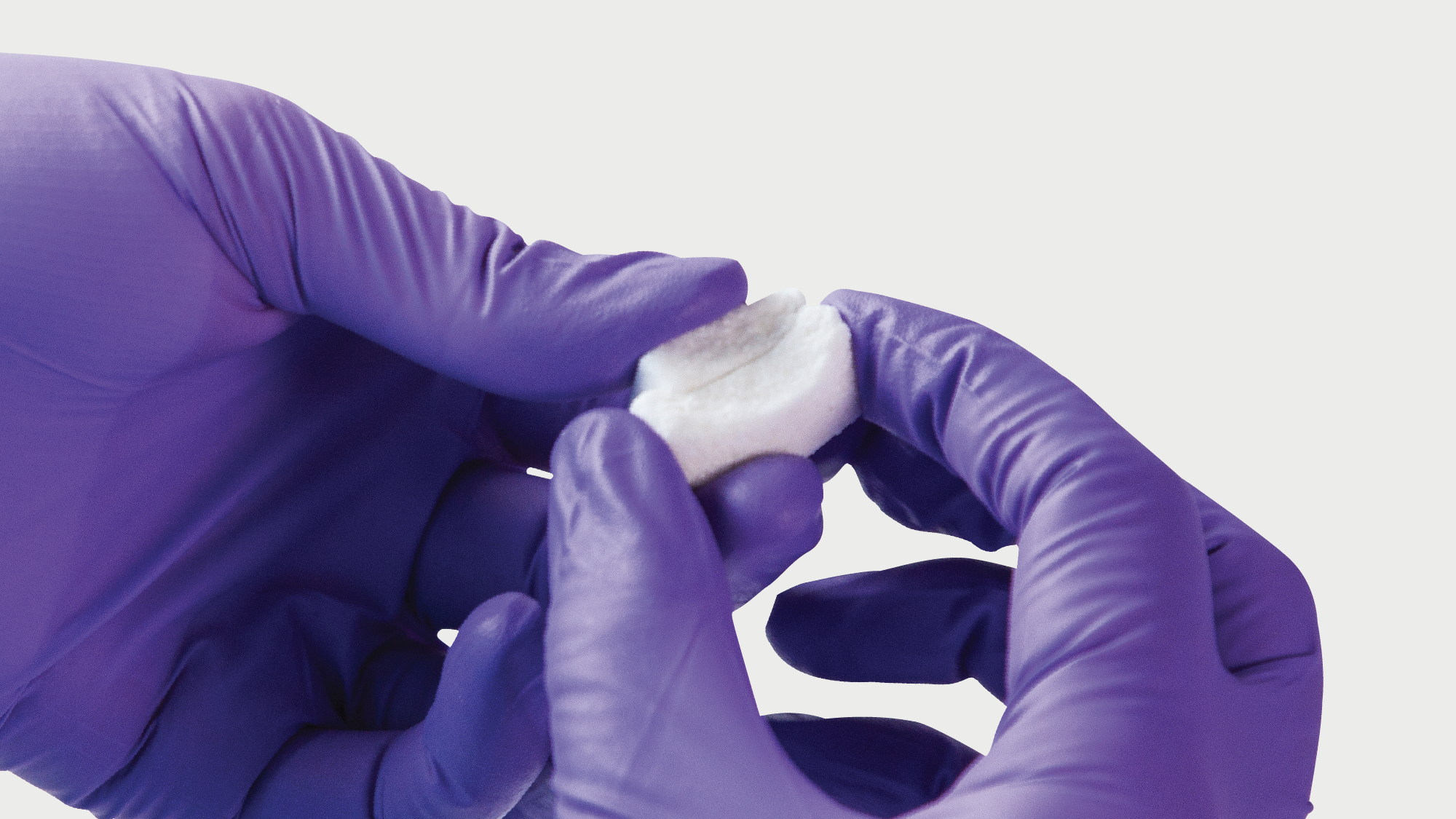
Attrax
Attrax Putty is now the first and only synthetic biologic to receive 510(k) clearance for use with thoracolumbar interbody systems. When used with Modulus XLIF interbody implants the combination of Attrax and Modulus resulted in a 97.8% rate of bone bridging20
Learn more about Attrax

Osteocel
Osteocel is a comprehensive bone graft developed to mimic the properties of a patient's own bone. Osteocel provides a complete and physiologic bone graft that contains all of the necessary components for bone growth: the cells, the signals, and the scaffold.
Learn more about Osteocel
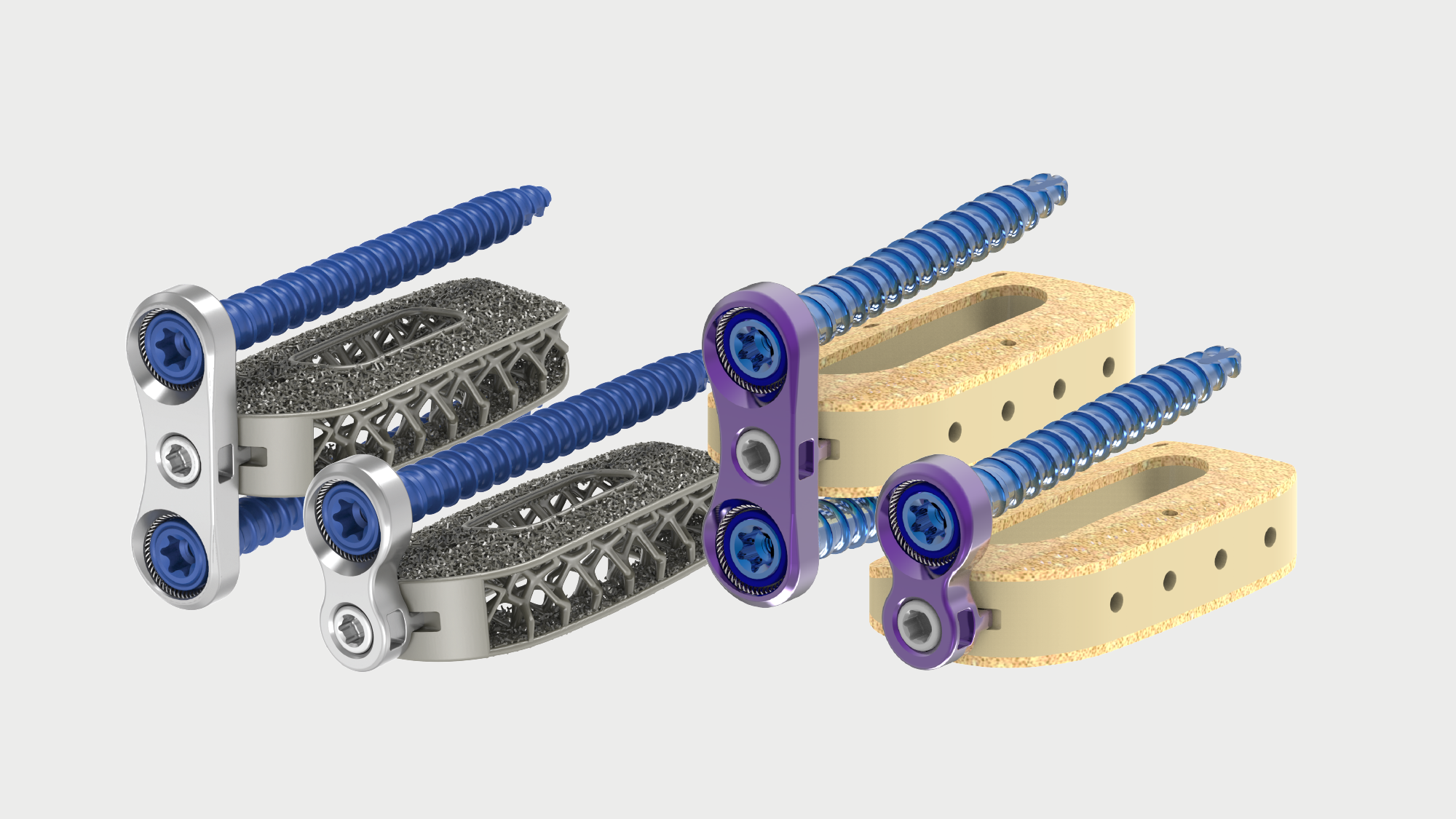
Modulus XLIF plate and Cohere XLIF AMS plate
Stability at the discretion of the surgeon, in multi-stage procedures or as standalone fixation. Simplified instrumentation allows the plates to be placed before or after insertion of the implant. The plates are available in single- and dual-sided options to best fit the surgeon and patient need.
Reline
Reline is the most comprehensive fixation system in spine, offering an easy-to-use yet powerful system. Reline delivers innovative technologies to support less invasive, open and hybrid techniques in a single seamless platform.

Pulse
Pulse is the first solution to integrate all the technologies required to enable better spine surgery into one single platform. Pulse integrates multiple enabling technologies, like neuromonitoring, patient-specific rod bending, smart imaging with radiation reduction and navigation to improve workflow, reduce variability and increase the reproducibility of surgical outcomes.

Neuromonitoring
Neuromonitoring with NVM5 is a foundational requirement in every XLIF case. Our services and technology provide proprietary automated nerve detection with standardized setup and clinically validated alerts21 to help reduce variability and allow for faster interpretation of neural information.

Patient-specific rod bending
The Bendini spinal rod bending system is used to create customized rods which are bent exactly to XLIF interbody implant locations. The system expedites manual rod manipulation via computer-assisted bend instructions.

Lessray
The use of X-ray imaging in MIS has greatly enhanced visualization. X-ray imaging is correlated with radiation exposure, which has been shown to have a negative impact on health through repeated exposure.22 The Lessray technology was designed to increase OR efficiency through streamlined imaging workflow, while also significantly reducing exposure to radiation for everyone in the room.23
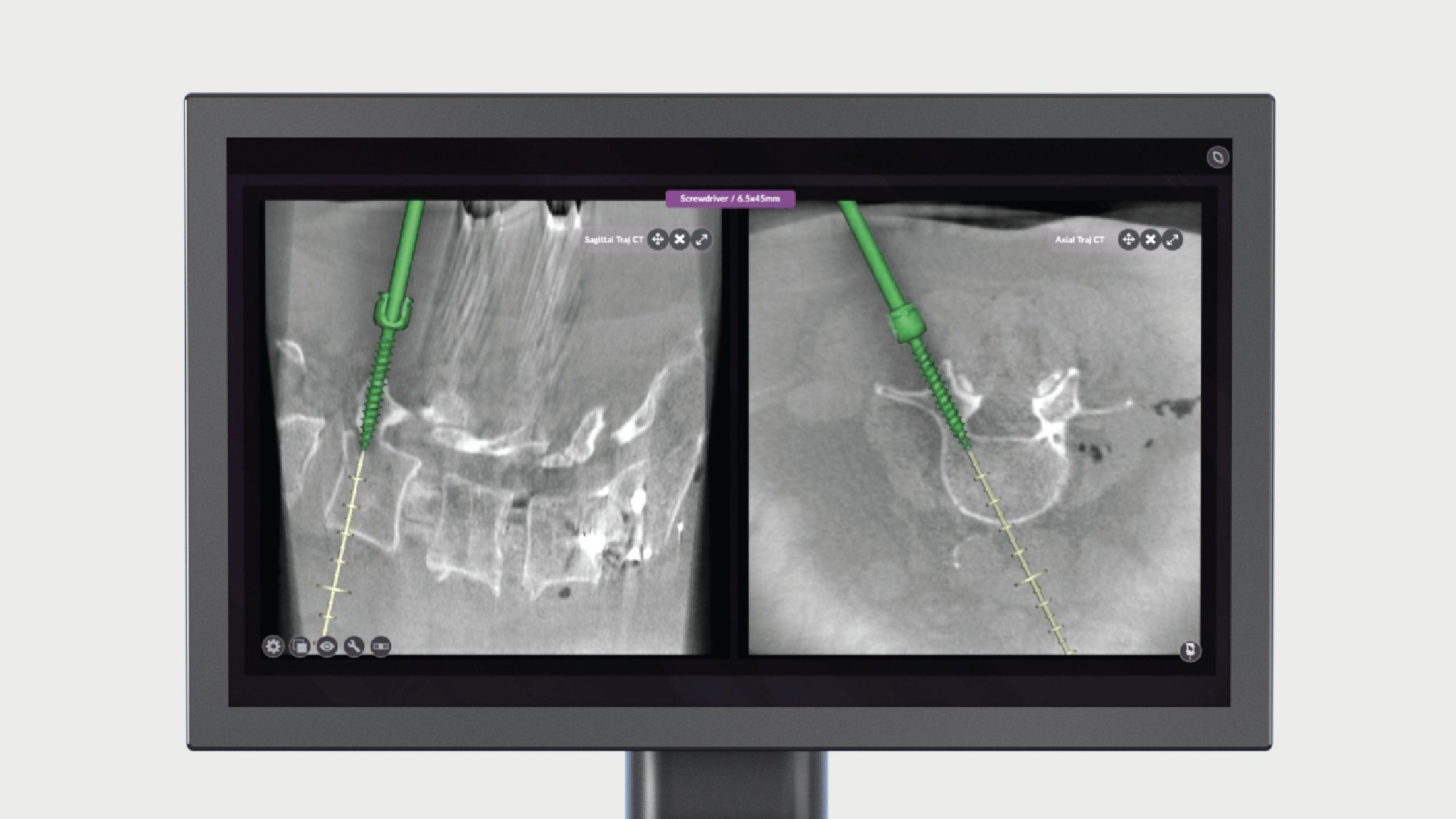
Navigation
Navigation in spine surgery offers the potential for more surgeons to adopt MIS techniques while improving implant accuracy and minimizing radiation. However, the complexity and time requirements of existing solutions have impeded adoption of navigation into the majority of spine surgeries. Pulse introduces a procedurally integrated navigation technology that features workflow technologies to improve ease-of-use and surgical efficiency in the OR.
Best-in-class education

By using modern medical education principles to elevate training programs of the past, CPD is able to support clinical education and practice development for participating surgeons.
Our competency-based courses provide peer-to-peer training, while obtaining valuable insights from real world scenarios, delivered by dedicated faculty members who are committed to providing an immersive education experience.
Expand your education on XLIF, XLIF Thoracic, XLIF Corpectomy and XLIF SPS.
1. Data on file.
2. Lehmen JA, Gerber EJ. MIS lateral spine surgery: A systematic literature review of complications, outcomes, and economics. Eur Spine J 2015;24(Suppl 3):287-313.
3. Cheng I, Briseno MR, Arrigo RT, et al. Outcomes of two different techniques using the lateral approach for lumbar interbody arthrodesis. Global Spine J 2015;5(4):308-14.
4. Khajavi K, Shen A, Lagina M, et al. Comparison of clinical outcomes following minimally invasive lateral interbody fusion stratified by preoperative diagnosis. Eur Spine J 2015;24(Suppl 3):322-30.
5. Okuda S, Miyauchi A, Oda T, et al. Surgical complications of posterior lumbar interbody fusion with total facetectomy in 251 patients. J Neurosurg Spine 2006;4(4):304-9.
6. Scaduto AA, Gamradt SC, Yu WD, et al. Perioperative complications of threaded cylindrical lumbar interbody fusion devices: anterior versus posterior approach. J Spinal Disord Tech 2003;16(6):502-7.
7. Sembrano JN, Tohmeh A, Isaacs R, et al. Two-year comparative outcomes of MIS lateral and MIS transforaminal interbody fusion in the treatment of degenerative spondylolisthesis: part I: clinical findings. Spine 2016;41(Suppl 8):S123-32.
8. Rodgers WB, Gerber EJ, Patterson JR. Fusion after minimally disruptive anterior lumbar interbody fusion: analysis of extreme lateral interbody fusion by computed tomography. SAS Journal 2010;4:63-6.
9. Gabel BC, Hoshide R, Taylor W. An algorithm to predict success of indirect decompression using the extreme lateral lumbar interbody fusion procedure. Cureus 2015;7(9):e317.
10. Lucio JC, VanConia RB, DeLuzio KJ, et al. Economics of less invasive spinal surgery: an analysis of hospital cost differences between open and minimally invasive instrumented spinal fusion procedures during the perioperative period. Risk Manag Healthc Policy 2012;5:65-74.
11. Dakwar E, Cardona RF, Smith DA, et al. Early outcomes and safety of the minimally invasive, lateral retroperitoneal transpsoas approach for adult degenerative scoliosis. Neurosurg Focus 2010;28(3):E8.
12. Dhall SS, Wang MY, Mummaneni PV. Clinical and radiographic comparison of mini-open transforaminal lumbar interbody fusion with open transforaminal lumbar interbody fusion in 42 patients with long-term follow-up. J Neurosurg Spine 2008;9(6):560-5.
13. Whitecloud TS, Roesch WW, Ricciardi JE. Transforaminal interbody fusion versus anterior-posterior interbody fusion of the lumbar spine: a financial analysis. J Spinal Disord 2001;14(2):100-3.
14. Preclinical data on file. Data may not be representative of clinical results. TR 9604787.
15. Evans NT, Torstrick FB, Lee CSD, et al. High-strength, surface-porous poly-ether-ether-ketone for load-bearing orthopedic implants. Acta Biomater 2015;13:159-67.
16. Evans NT, Torstrick FB, Safranski DL, et al. Local deformation behavior of surface porous polyether-ether-ketone. J Mech Behav Biomed Mater 2017;65:522-32.
17. Torstrick FB, Lin ASP, Potter D, et al. Porous PEEK improves the bone-implant interface compared to plasma-sprayed titanium coating on PEEK. Biomaterials 2018;185:106-16
18. Smith WD, Dakwar E, Le TV, et al. Minimally invasive surgery for traumatic spinal pathologies: a mini-open, lateral approach in the thoracic and lumbar spine. Spine 2010; 35(26 Suppl): S338-S346.
19. 2. Pekmezci M, McDonald E, Kennedy A, et al. Can a Novel Rectangular Footplate Provide Higher Resistance to Subsidence When Compared to Circular Footplates?: An Ex Vivo Biomechanical Study. Spine 2012; In Press.
20. Malone, H., Mundis, G. M., Jr., Collier, M., Kidwell, R. L., Rios, F., Jelousi, M., Galli, S., Shahidi, B., Akbarnia, B. A., & Eastlack, R. K. (2022). Can a bioactive interbody device reduce the cost burden of achieving lateral lumbar fusion?, J Neurosurg Spine (published online ahead of print 2022). Retrieved Oct 18, 2022
21. Tohmeh AG, Rodgers WB, Peterson MD. Dynamically evoked, discrete-threshold electromyography in the extreme lateral interbody fusion approach. J Neurosurg Spine 2011;14(1):31-7.
22. Vano E, Kleiman NJ, Duran A, et. al. Radiation-associated lens opacities in catheterization personnel: results of a survey and direct assessments. J Vasc Interv Radiol 2013;24(2):197-204.
23. Wang TY, Farber SH, Perkins SS, et al. Internally randomized control trial of radiation exposure using ultra-low radiation imaging versus traditional C-arm fluoroscopy for patients undergoing single-level minimally invasive Transforaminal lumbar Interbody fusion. Spine 2017;42(4);217-23.


