Modulus® Titanium Technology
Unlike any other 3D printed titanium implant on the market, Modulus is designed through a proprietary optimization algorithm that balances strength and radiolucency.
Unlike any other 3D printed titanium implant on the market, Modulus is designed through a proprietary optimization algorithm that balances strength and radiolucency.
Adhering to the three core principles of Advanced Materials Science—Surface, Structure, and Imaging—NuVasive has pioneered design and manufacturing methods that combine the inherent benefits of porosity with the advantageous material properties of titanium to create implants intelligently designed for fusion.
<- Swipe to view more ->
Porosity elicits a significantly stronger osteogenic response at the cellular level compared to roughened or nano-roughened surfaces2-5 on their own.
Fully porous endplate design promotes new bone on-growth and in-growth,1 demonstrating the greatest integration strength by 12 weeks compared to alternative implant materials.1
Microporous endplate architecture maximizes bone-to-implant contact, increasing expulsion resistance.6
The increased surface area and wicking capability of the porous surface improves blood to implant contact compared with traditional interbody implants.
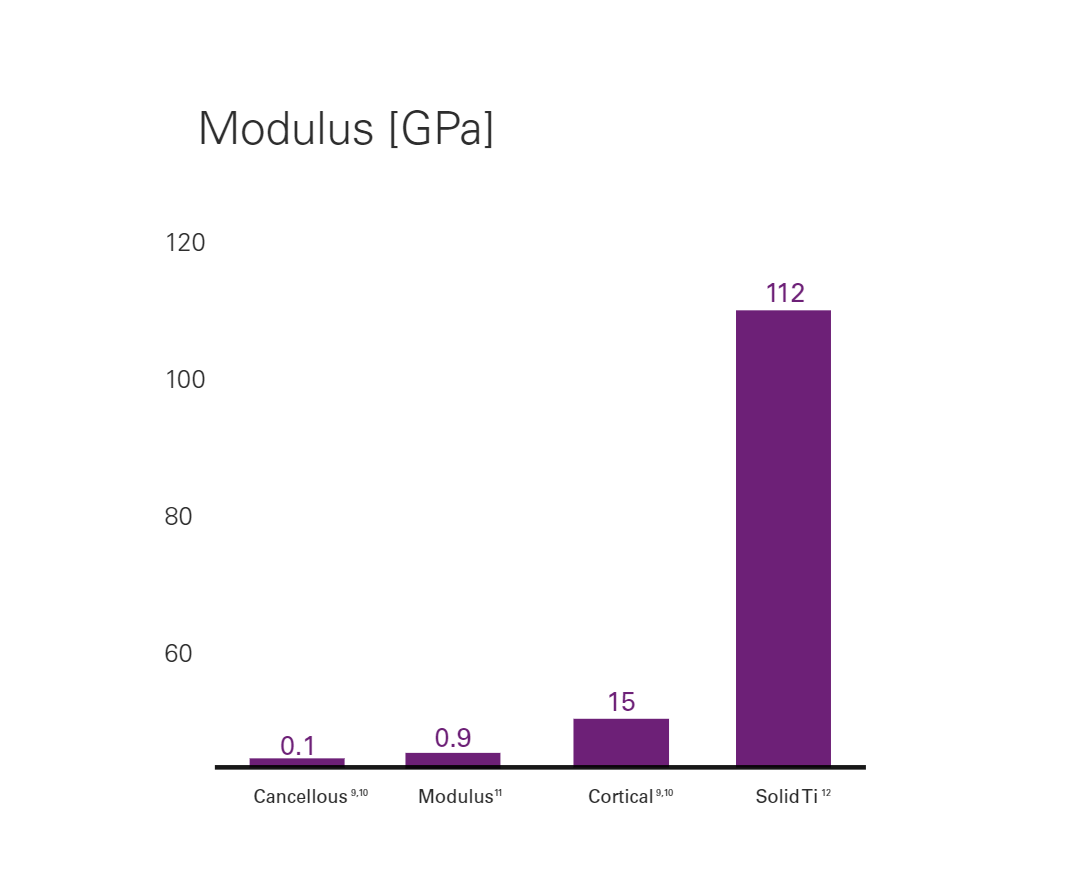
Implants are designed with an optimized balance between strength and stiffness so as to minimize stress shielding7 and subsidence.8
Modulus implants implement a proprietary design optimization methodology, generating a unique internal architecture for a desired effective modulus that is similar to bone.
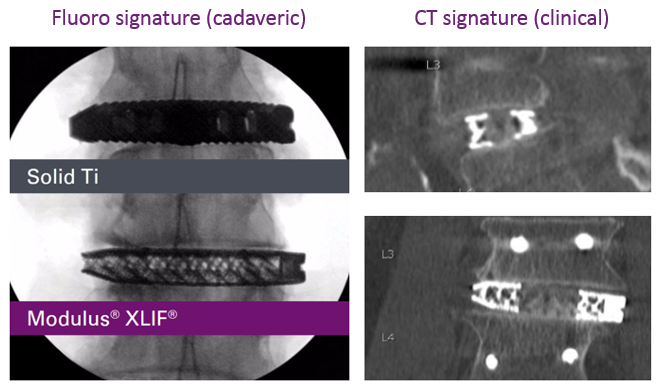
Created with imaging clarity in mind, the proprietary implant design and manufacturing process allow enhanced visualization on a variety of imaging modalities.
1 Preclinical data on file; data may not be representative of clinical results. TR 9604787. 2 Cheng A, Humayun A, Cohen DJ, et al. Additively manufactured 3d porous ti-6al-4v constructs mimic trabecular bone structure and regulate osteoblast proliferation, differentiation and local factor production in a porosity and surface roughness dependent manner. Biofabrication 2014;6:045007. 3 Cheng A, Humayun A, Boyan BD, et al. Enhanced osteoblast response to porosity and resolution of additively manufactured ti-6al-4v constructs with trabeculae-inspired porosity. 3D Print Addit Manuf 2016;3:10-21. 4 Cheng A, Cohen DJ, Kahn A, et al. Laser sintered porous ti-6al-4v implants stimulate vertical bone growth. Ann Biomed Eng 2017;45:2025-35. 5 Cheng A, Cohen DJ, Boyan BD, et al. Laser-sintered constructs with bio-inspired porosity and surface micro/nano-roughness enhance mesenchymal stem cell differentiation and matrix mineralization in vitro. Calcif Tissue Int 2016;99:625-37. 6 Preclinical data on file. Data may not be representative of clinical results. TR 9603905. 7 Chatham LS, Patel VV, Yakacki CM, et al. Interbody spacer material properties and design conformity for reducing subsidence during lumbar interbody fusion. J Biomech Eng 2017;139(5):051005. 8 Preclinical Data on File; data may not be representative of clinical results. TR 9603972.9 Hou FJ, Lang SM, Hoshaw SJ, et al. Human vertebral body apparent and hard tissue stiffness. J Biomech 1998;31(11):1009-15. 10 Ladd AJ, Kinney JH, Haupt DL, et al. Finite-element modeling of trabecular bone: Comparison with mechanical testing and determination of tissue modulus. J Orthop Res 1998;16(5):622-8. 11 Preclinical data on file. Data may not be representative of clinical results. TR 9604781. 12 Elias CN, Lima JH, Valiev R, et al. Biomedical applications of titanium and its alloys. JOM 2008;60(3):46-9.